Brisbane North PHN
Year in Review 2023-24

A message from our CEO and Chair
Our shared vision, as CEO and Chair of Brisbane North PHN and as an organisation, is a community where good health is available to everyone.
Delivering coordinated, high quality, patient-centred health and community care services across a diverse urban and regional landscape to a population over a million strong is no small task, and yet we're proud to report –
79,000 people across our region received a Brisbane North PHN commissioned service in 2023-24.
This number, thanks to the strength of our partnerships and commissioning efforts, is compared to the 33,000 community members serviced last year. We have, in the spirit of capacity building and echoing the theme of our 2024 Metro North Health Forum, this year truly built momentum.
We understand more than ever that working together is always more effective than working in silos.
Working together with our Board, who bring together a wealth of local knowledge and experience in primary healthcare to chart a course towards excellence.
Working together with our Health and Hospital Service (HHS) partner, Metro North Health, to deliver collaborative regional governance. The Health Alliance, the strategic cornerstone of this partnership, continues to demonstrate the impact that shared models of care can deliver.
Working together with and for our vulnerable communities, ensuring we remain informed by their voices. In partnership with the Institute of Urban Indigenous Health (IUIH), our PHN and HHS along with others from across South-East Queensland continue to champion new ways of working towards more inclusive and culturally responsible models of care. The joint Health Equity Strategy represents a collaborative approach to achieving “one system” reform and health equity for our First Nations people.
Working together with our valued commissioned service providers, primary healthcare partners and stakeholders who, collectively, have helped us this year to deliver over 367,000 procured service contacts.
Represented in this number are the individual stories of everyone who visited a Safe Space when in emotional distress, received fast and convenient treatment at a Medicare Urgent Care Clinic, was able to better navigate the aged care system with the support of a care finder, or who connected with a Link Worker in a time of loneliness and need. We are pleased to share some of these stories, and those from other PHN-commissioned programs, with you in the report below.
And finally, working together within and across our program teams. It’s our PHN people who have fostered the innovative and collaborative approaches that have seen us successfully deliver these improved outcomes in our communities, to those who need it the most.
2025 will see us deliver the Joint Regional Needs Assessment (JRNA) with Metro North Health – a new, shared approach to understanding the unique health, wellbeing and social needs of our shared communities.
Our achievements as an organisation – this year, and every year – are underpinned by the mutual trust, respect and vision we share with exceptional providers and partners to achieve the best for our community.
– Libby Dunstan, PHN CEO



A new strategic roadmap
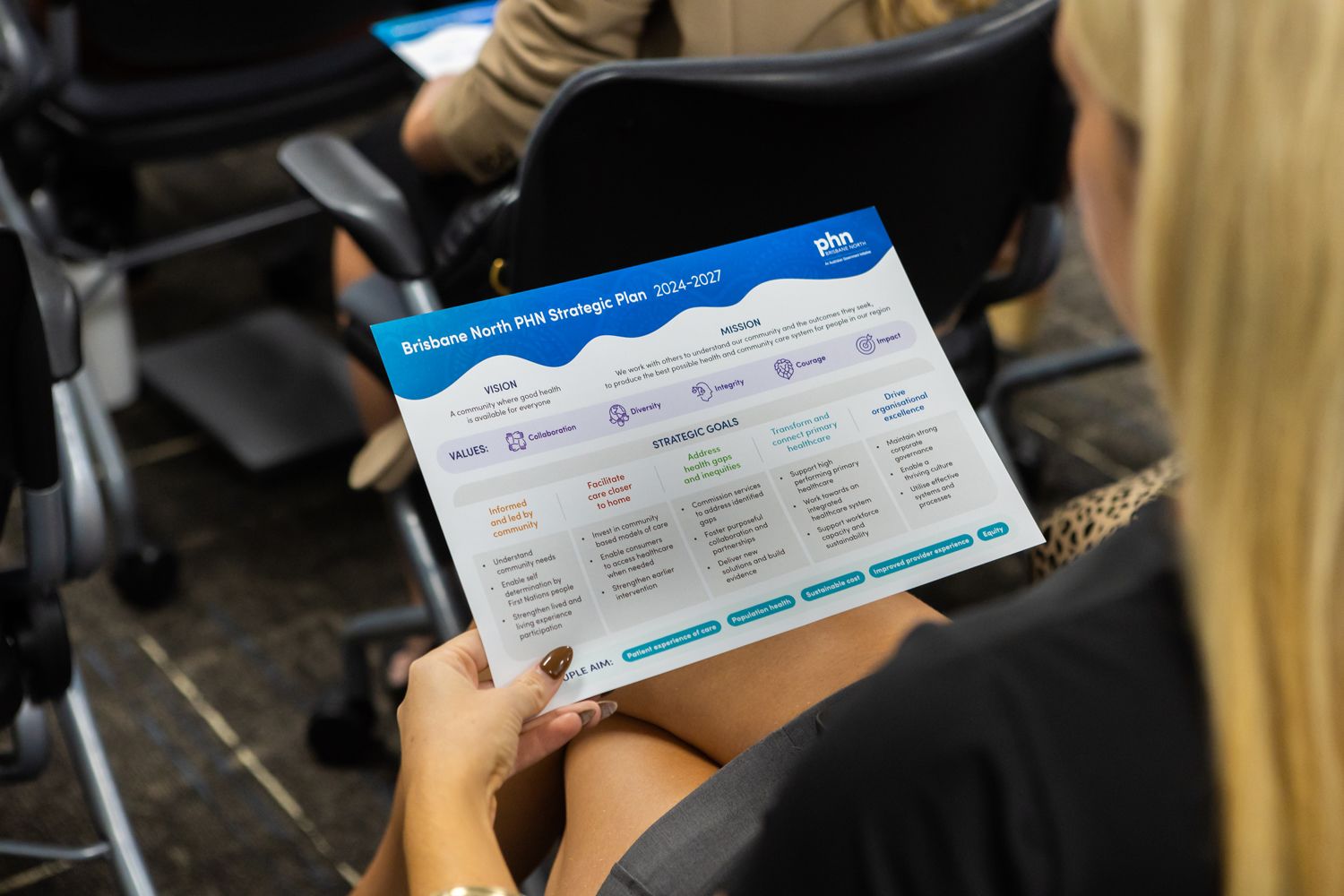
In 2023, the Brisbane North PHN Board commenced a review of our Strategic Plan that aimed to maximise organisation success, and reflect and respond to new opportunities and challenges.
This was a highly consultative process that sought out, and was informed by, the voices and insights of both internal and external stakeholders who offered an enriched and deepened understanding of our community's needs.
While our vision and values remain unchanged, the refreshed 2024-2027 Plan delivers an updated mission and five reframed and refocused strategic goals to work towards. Each of these goals, outlined below, represents a chapter of our 2023-24 Year in Review.
We are emphatic about the ambition, integrity and courage with which our PHN will pursue these goals over the coming years.
– Libby Dunstan, PHN CEO
Download Brisbane North PHN's 2024-2027 Strategic Plan.
Read more about its launch.
A deep reflection of who we are and where we're going.
Dr Jennifer Schafer, PHN Board Chair
Address health gaps and inequities

Core to our role as a commissioning organisation, this year we have added a strategic goal that seeks to address health gaps and inequities by:
Commissioning services to address identified gaps |
Fostering purposeful collaboration and partnerships |
Delivering new solutions and build evidence.
Two multidisciplinary endometriosis and pelvic pain clinics commenced specialist care for women and people assigned female at birth from Neighbourhood Medical at Bardon, and for Aboriginal and Torres Strait Islander women at Moreton Aboriginal and Torres Strait Islander Community Health Service (MATSICHS). Over 200 patients – 80 per cent of whom reported receiving excellent care – have been through Neighbourhood Medical’s doors since September 2023.
This experience has surpassed my expectations - the doctor and nurse have helped me beyond measure. Incredible and life-changing service.
– EPP clinic consumer
As more people choose to call our region home, demand on our local hospitals has increased. In continuing efforts to relieve critical capacity in emergency departments (EDs) by enhancing access to after-hours services, two new Medicare Urgent Care Clinics (UCCs) were commissioned to provide timely, episodic care, closer to home at Murrumba Downs and Northside (Kedron).
Since opening in October 2023 and February 2024 respectively, both clinics have been delivering exceptional care to patients like Jacinda. Pictured with her mother, Karen, Jacinda was able to relay her positive treatment experience at Murrumba Downs Medicare UCC to Prime Minister the Hon. Anthony Albanese this February when he officially launched and toured the facility with Queensland Premier Steven Miles, Minister for Health and Aged Care the Hon. Mark Butler, Senator the Hon. Anthony Chisholm and Senator the Hon. Murray Watt.
On average 680 individuals per year are receiving services from one of three PHN-commissioned Mental Health Hubs, which combine clinical and non-clinical services to facilitate access to tailored packages of mental healthcare for those with acute mental illness. Findings show this integrated model of care is working to support these members of our community – hub patrons reported improved recovery outcomes, and that the psychosocial support they received was highly valued.
Safe Spaces and newly established Compassionate Villages provide a critical stop-gap service for those in emotional distress. For these people, for whom an emergency department may not be the best intervention, the Safe Space network continues to provide non-clinical respite, warm peer support, and a safe place to land. Our guest demographics told us that the service is inclusive, culturally safe and identity affirming, including for those who identify as Aboriginal and Torres Strait Islander, LGBTIQAP+ or as being from a culturally and linguistically diverse background.
The PHN will continue to commission mental health services for the remote communities of Norfolk Island through to 2026, and is actively continuing development for a new partnership between the Institute for Urban Indigenous Health (IUIH) and headspace to provide further First Nations mental health and wellbeing services.
Protecting our most vulnerable people and communities
The expansion of our annual series of COVID and flu vaccine clinics to include a third vulnerable region is helping our PHN to improve critical vaccine coverage in the communities with the highest need.
295 vaccines to 206 patients
across three community vaccine clinics in Kilcoy, Caboolture and Woodford.
Informed and led by community voice

We remain informed and led by community voice, and have strongly called out our commitment to:
Understand community needs |
Enable self-determination by First Nations people |
Strengthen lived and living experience participation.
Our newly convened Mental Health Strategy and Partnerships portfolio has continued to undertake the critical work of embedding Lived Experience (LE) into PHN core business.
Read more: Planning for Wellbeing: a human-centred approach to mental healthcare.
The Crisis Reform Project, a joint initiative of Metro North Mental Health and the PHN, was established to scope, co-design and deliver a strategy with clear vision for crisis reform for our region.
Work to reduce the incidence of suicide across this shared region was also progressed by the newly formed Brisbane North and Moreton Bay Suicide Prevention Collaborative. Membership from across sectors – including health, research, NGOs, emergency services, disability, education, local government and community organisations – comprising a range of backgrounds including First Nations, people with lived and living experience, veterans, culturally and linguistically diverse and LGBTIQAP+, ensures the Collaborative can undertake coordinated efforts using evidence-based strategies.
Over 20,000 people in our region identify as Aboriginal or Torres Strait Islander, and a large proportion of these people are living in the most disadvantaged areas of our region. In August 2023, our Board issued a resolution in support of the Voice to Parliament that recognised the need for, and committed our further action to, ensuring and securing self-determination of First Nations people in our region and across Australia.
Several new internal frameworks – from our Engagement and Partnering Framework, Toolkit and related Community of Practice, to continuing work to establish our Equity and Access Framework – have helped to empower our PHN’s people to act as best practice partnership brokers in their engagement with stakeholders, community members and consumers, and to keep the tenets of health equity front of mind when doing so.
We are pleased that in a post-COVID world we are again able to bring our aged care workforce together face-to-face several times per year in continued pursuit of strengthening aged care quality standards and access to (better and primary) care for residents living in Residential Aged Care Homes.
As a PHN, we are committed to supporting and enabling culturally responsive, inclusive and partnership-centred solutions and models of care that uphold the unique rights of Aboriginal and Torres Strait Islander people. We are committed to listening to, meaningfully engaging with, and strengthening First Nations voices.
Brisbane North PHN Board of Directors, in
support of the Voice to Parliament 2023
Engaging valued stakeholders to build a better health and community care system
As lead and member agency on a range of Committees and Consortiums, we understand and partner on the foundation that better health outcomes are achieved through collaboration.
35 Collaboratives with over 350 members
47 engagement events with 1196 attendees. 84 training events with 1033 attendees.
Facilitate care closer to home

Invest in community-based models of care |
Enable consumers to access healthcare when needed |
Strengthen earlier intervention
The top ten per cent of general practice patients account for up to half of all appointments, and many often have unmet social, emotional or other wellbeing needs. We’ve recognised that a medical approach alone is not sufficient – instead, we need to pioneer new place-based and community-led solutions that will enable us to make system changes, from the individual and up.
Four new programs under the umbrella of a holistic Early Interventions Project, which includes intergenerational and First Nations streams, have seen our Healthy Ageing and Team Care Coordination (TCC) teams work together with partners from IUIH, Footprints, Communify, Micah Projects, Ozcare and others to commission services to support healthy ageing and the ongoing management of chronic conditions to promote independence and better quality of life for participants.
Read more: Generational health: finding care and fostering connection in our communities.
One such program, Social Health Connect (SHC), is facilitated by Footprints Community to employ social prescribing for adults in the Kilcoy and Caboolture regions. This non-clinical initiative seeks to counter the effects of loneliness and social isolation by connecting people to their communities, and the people, services and activities within them.
I talk about Footprints with a lot of people and say… it has changed my life.
– Debbie, Footprints SHC consumer
The collaborative PHN and Metro North Health Starting Well initiative is enhancing ante and postnatal care through better access to maternity services for vulnerable mums and newborns in the Caboolture region. The program is facilitating better health outcomes for both mother and baby – 91 per cent of Starting Well babies are born at full-term and at a healthy weight, and healthcare appointment attendance is increased.
As a first-time mum or during any pregnancy, Starting Well is a safe space linking me to the appropriate services I need.
– Ashlee Corlett and baby Arlo, Starting Well mum
Team Care Coordination (TCC) and the Regional Assessment Service (RAS) continue to increase their referral capacity year on year. In 2023-2024, TCC supported more than 2,000 people with complex or chronic health conditions to live well, in their homes, their way.
Other transformative projects championing integrated models of care have gained momentum, including ASPIRE, a collaborative and systems approach to improving medication safety, and PainWISE, a community-based approach to supporting people with persistent pain. The PHN remains committed to supporting vulnerable groups and reducing frequent ED presentations via the Working Together to Connect Care program, funded under Metro North Connected Community Pathways.



Improving access to primary care in the community
Medicare UCCs are a new model of care, designed to provide people with more options for care that is urgent, unplanned or required after-hours. Our Medicare UCCs are staffed by doctors and nurses, and assisting to reduce pressure on our local EDs.
13,984 episodes of care
delivered to 11,814 people at a Medicare Urgent Care Clinic (UCC) in our region.
Transform and connect primary care

Support high performing primary healthcare |
Work towards an integrated healthcare system |
Support workforce capacity and sustainability.
Through our Primary Care team’s Practice Support function, we supported 295 general practices to access Strengthening Medicare GP Grant funding, a new flagship website and ongoing Continuous Quality Improvement (CQI) initiatives to foster innovative practice and enhanced service delivery.
The success of the Health Alliance’s Care Collective program, which has supported more than 446 clients living with complex and chronic health conditions in the Caboolture region to date, saw it expanded to general practice patients in the Redcliffe region. The Care Collective have remained committed to supporting the ongoing professional development of our growing network of nurse Complex Care Coordinators.
Read more: From complex to collaborative: a collection of consumer and coordinator stories from the care Collective.
While significant work progressed to better equip our general practice and pharmacy workforce to deliver high quality palliative care at home and in the community, other primary care projects came to an end.
The Bribie Island After-Hours Pilot ceased operation from Banksia Doctors in June 2024 after 20 months of service. The clinic saw over 1,400 patients who may not otherwise have been able to seek general practice treatment, offering an invaluable community service prior to the opening of the Bribie Island Satellite Hospital a month later.
The GP Workforce Planning and Prioritisation (GP WPP) local and Shared Service teams have continued to engage and build strong rapport with GPs, registrars and practices across our region, having now consolidated the critical insights of these stakeholders into Workforce Needs and Training Capacity Reports Two and Three which continue to help inform the future of Australia’s GP workforce.
Strong uptake of voluntary patient enrolment via MyMedicare by GPs, practices and patients across our region continues to strengthen our conviction as an organisation that patient-centred care is the way forward for our health system.
Dr Jennifer Schafer, PHN Board Chair and GP
Supporting clinicians to support our communities
The Initial Assessment and Referral (IAR) is a decision support tool that assists GPs and other referrers to find the most suitable level of care for patients presenting with mental health distress or concerns. It provides a standardised, evidence-based and objective approach to assist with determining appropriate mental healthcare service and support recommendations.
321 GPs trained across 47 sessions
in the Initial Assessment and Referral decision support tool (IAR-DST) to structure mental health consultations and help provide appropriate interventions for patients presenting to primary care in distress.
Drive organisational excellence

As always, we drive organisational excellence to enable us to achieve our strategic goals by:
Maintaining strong corporate governance |
Enabling a thriving culture |
Utilising effective systems and processes.
The implementation of an organisation-wide Clinical Governance Framework has ensured our PHN people are engaged with a systematic approach to providing safe, effective, high-quality, person-centred consumer care.
Brisbane North PHN proudly passed our ISO 9001 and ISO 27001:2022 (Information Security Management System) recertifications, reflecting our unwavering dedication to data security, operational excellence, and continuous improvement.
In the further pursuit of ensuring our work is built on a foundation of data-driven decisions, the PHN has also become a prescribed entity of Queensland Health to improve data sharing opportunities.
Our Joint Protocol with Metro North Health, which formalises and provides shared governance around ways of working together, was reviewed and renewed for another three-year cycle.
Work on our triennial 2024-2027 Health Needs Assessment (presently transitioning to a Joint Regional Needs Assessment in partnership with Metro North Health) continues to inform and ensure that the procurement, implementation and evaluation of health services and programs across our shared region remain evidence based and tailored to our community’s needs.

Special thanks to
Brisbane North PHN and Metro North
Health's GP Liaison Officer (GPLO) Program

Producing the best possible system of care for the people of our region.
79 per cent of $92.9 million in grant income commissioned out to providers directly servicing our communities.
367,000
PHN commissioned service contacts delivered.
A community where good health
is available to everyone
Impactful stories from the programs we commission across the North Brisbane and Moreton Bay region.
Planning for Wellbeing: a human-centred approach to mental healthcare
A human-centred design approach to regional planning is shaping the new iteration of the North Brisbane and Moreton Bay Joint Comprehensive Regional Plan for Mental Health and wellbeing - one that is responsive to community feedback and focused on increasing connection across our communities and between service providers.
Generational health: finding care and fostering connection in our communities
Following the passing of her late husband, Beverley, 88, found herself living alone with dementia. Daughters Rhonda and Pam share how their mum has taken to the Paper Planes Intergenerational Play Program with gusto and how Bev's "days are brighter" since joining the program.
From complex to collaborative: a Care Collective of consumer and coordinator stories
After being diagnosed with Congestive Heart Failure (CHF), Gloria withdrew from the activities she loved in fear of what might happen to her health. After referral to the Health Alliance’s flagship Care Collective program, Gloria set out to take back her heart, her health and her life.
Towards better health outcomes, together
See our year in numbers, key milestones and highlights from our program teams by downloading the full Year in Review.













